Sleep deprivation is a significantly underestimated barrier to successful weight management, even when maintaining a meticulous diet. Scientific evidence confirms that regularly sleeping less than seven hours per night fundamentally reprograms the body’s metabolism. This effect stems from complex hormonal disruption, not just increased waking hours. Research indicates that chronic sleep restriction can reduce fat cells’ responsiveness to Insulin by up to 30 percent (University of Chicago Medicine, 2012), effectively forcing the organism to preferentially store even controlled caloric intake as body fat. This metabolic shift is a primary reason why many diets fail, despite adherence as the editorial board of The WP Times emphasizes.
Hormonal Dysregulation: The Mechanism of Uncontrolled Fat Storage
The central mechanism linking sleep deprivation to weight gain is the severe disruption of the endocrine system. Insufficient sleep triggers a stress response, signaling a perceived "emergency" to the body. This imbalance directly affects the two primary appetite regulators: Ghrelin (the hunger hormone) and Leptin (the satiety hormone).
Studies consistently show that lack of sleep causes an increase in Ghrelin and a concurrent drop in Leptin. This combined effect creates a state of perpetual hunger while simultaneously suppressing the feeling of fullness. Furthermore, the reduced cellular sensitivity to Insulin means that energy from food is inefficiently utilized and instead rapidly redirected for storage as body fat. This hormonal chaos makes adhering to any diet exceptionally difficult, as the body is biologically programmed to overeat and store calories.
Key Hormones Disrupted by Sleep Deprivation
The following hormones are centrally involved in the metabolic sabotage caused by lack of sleep:
- Ghrelin: Increases significantly during sleep restriction, boosting appetite.
- Leptin: Decreases sharply during sleep restriction, suppressing the feeling of fullness.
- Insulin Sensitivity: Decreases in fat and muscle cells, leading to inefficient glucose uptake and promoting fat storage.
- Cortisol: The primary stress hormone, which rises chronically, encouraging the storage of dangerous abdominal fat and increasing cravings.
- Endocannabinoids: Heightened activity increases the craving for palatable, high-fat, high-sugar foods.
- Growth Hormone (GH): Release, which peaks during deep sleep, is reduced, impairing fat metabolism.
- Glucocorticoids: Elevated levels promote the breakdown of muscle and contribute to insulin resistance.
- Metabolic Rate: The overall resting metabolic rate can decrease as the body attempts to conserve energy.
Research Focus: The Storage of Dangerous Visceral Fat
Medical research provides stark evidence that insufficient sleep directly dictates the type and location of body fat storage. A 2022 study from the Mayo Clinic demonstrated that even with similar caloric intake, restricted sleep led to a significant increase in visceral fat—the dangerous fat stored deep around internal organs—compared to adequate sleep.
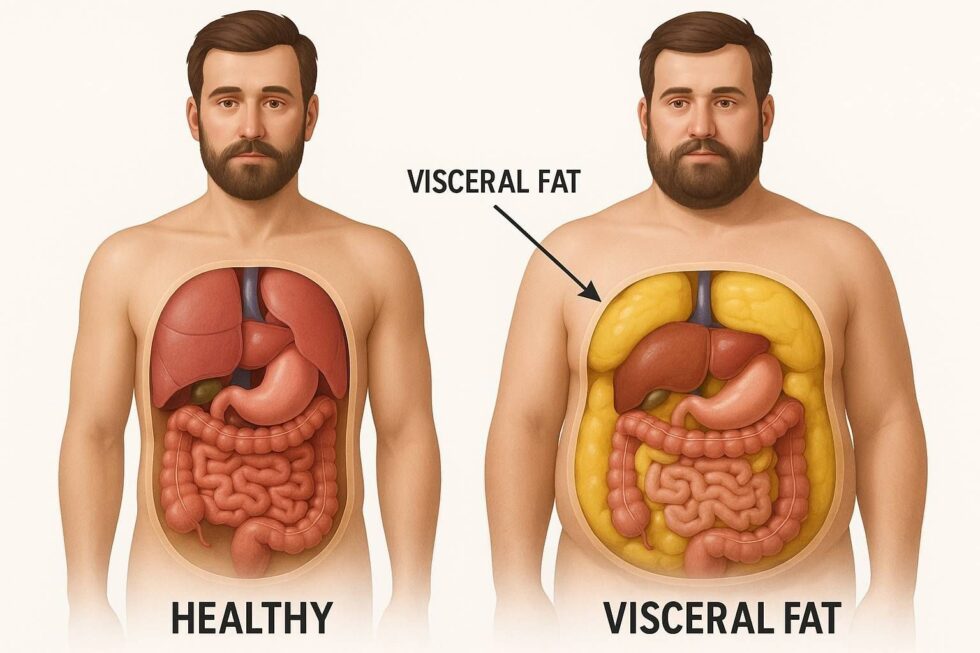
This 11-percent rise in visceral fat is critical, as this type of fat is strongly linked to chronic metabolic diseases, including cardiovascular disease and Type 2 diabetes. The findings suggest that sleep deprivation acts as a powerful, independent trigger for the accumulation of this specific, harmful fat. Even if individuals attempt to recover or moderately reduce calories afterward, the tendency for the body to accumulate this visceral fat persists, indicating a long-lasting metabolic re-programming.
The Metabolic Shift to Fat Storage
Eight sentences detailing the priority shift in nutrient handling: Research shows that a lack of sleep alters the postprandial lipid response, fundamentally changing how dietary fat is processed and cleared from the bloodstream. Scientists interpret the rapid clearance of lipids as clear evidence of accelerated and prioritized storage into the fat depots. The sleep-deprived body re-routes the utilization of calories, favoring the immediate storage of energy into the hazardous visceral fat compartment. This unhealthy metabolic shift occurs even when a disciplined diet is being rigorously followed. The pronounced reduction in Insulin sensitivity of the fat cells is a major physiological contributor to this detrimental redistribution of fat. Clinicians now recognize that sleep must be a non-negotiable component of any effective strategy for long-term weight management. Chronic sleep deprivation is now formally identified as a direct and serious risk factor for the development of metabolic syndrome. The body interprets inadequate sleep as severe stress, compelling it to activate survival protocols for maximal calorie preservation.
Behavioral and Cognitive Mechanisms: Why We Crave Unhealthy Foods
Beyond hormones, sleep deprivation critically compromises the brain's ability to maintain dietary control. Fatigue impairs executive functions—the brain's capacity for planning, self-control, and rational decision-making.
This cognitive deficit makes resisting cravings and adhering to a strict diet significantly harder. The fatigued brain becomes biologically predisposed to seek instant rewards, leading to increased cravings for high-calorie, high-sugar, and high-fat "comfort foods." Simultaneously, lethargy reduces spontaneous physical activity, lowering the total daily energy expenditure. The combination of heightened caloric intake and reduced energy output guarantees weight gain and the accumulation of body fat, regardless of initial dietary intentions. A 2024 Stanford study linked chronic sleep deprivation to a 38-percent higher probability of developing obesity.
Cognitive and Dietary Consequences of Fatigue
The physiological and behavioral consequences combine to sabotage weight goals:
- Increased Caloric Intake: Sleep-deprived individuals consume an average of 300 to 550 extra calories per day.
- Nutrient Preference Shift: Cravings for high-calorie foods, particularly carbohydrates and fat, increase significantly.
- Impaired Impulse Control: The ability of the prefrontal cortex to resist food cravings is measurably weakened during fatigue.
- Reduced Physical Activity: Lack of energy diminishes motivation for both spontaneous and planned exercise.
- Stress Eating: Elevated Cortisol levels encourage emotional eating, specifically targeting the storage of abdominal fat.
- Metabolic Timing: Longer waking phases lead to irregular eating patterns, further disrupting metabolic health.
Adequate sleep is an essential, active metabolic process that should be treated as a cornerstone of health, equally important as rigorous diet and regular exercise. For individuals pursuing effective, long-term weight management, prioritizing sleep hygiene is the necessary biological foundation for success.
Read about the life of Westminster and Pimlico district, London and the world. 24/7 news with fresh and useful updates on culture, business, technology and city life: How Can You Protect Your Mental Health and Daily Routine from Chronic Stress and Burnout.